By Sophie Davis-Cooper on April 29, 2021
In response to the COVID-19 pandemic, the necessity to reduce face-to-face consultations and deliver care safely to vulnerable patients in their own homes has driven remote patient monitoring into the limelight. While this way of managing patients existed a long time before the pandemic, healthcare providers and patients have never been more open-minded to embracing this form of digital health technology.
Although remote monitoring brings many benefits, from reducing emergency hospital admissions to significant cost savings, there are a number of concerns that healthcare providers often need to address before adopting this modern care model.
We have listed the top 6 potential barriers to remote patient monitoring and how we help clinicians and patients beat them.
1. I don’t have time to use another system
When you hear the phrase ‘remote patient monitoring system’ your first thought might be ‘that’s more work for me’.
We understand the idea of using a new system can be daunting, but our clinical evidence and years of experience have shown that remote monitoring makes clinicians’ work more efficient, not more time consuming. By working closely with clinical teams, we ensure the monitoring system is quick and simple to use, while saving clinicians precious time.
In a case study on triaging patients in real-time with remote monitoring, the GP Clinical Lead at Rushey Mead Health Centre, Dr Amit Rama noted:
“CliniTouch Vie asks the resident all the questions beforehand, which can make the consultation a lot quicker and more effective, giving me time back for care where it’s most needed. I have an average of 3 hours allocated to review patients from both care homes one day a week, and since using CliniTouch Vie, which highlights which patients have an acute problem to review, I am saving an estimated half an hour per care home.”
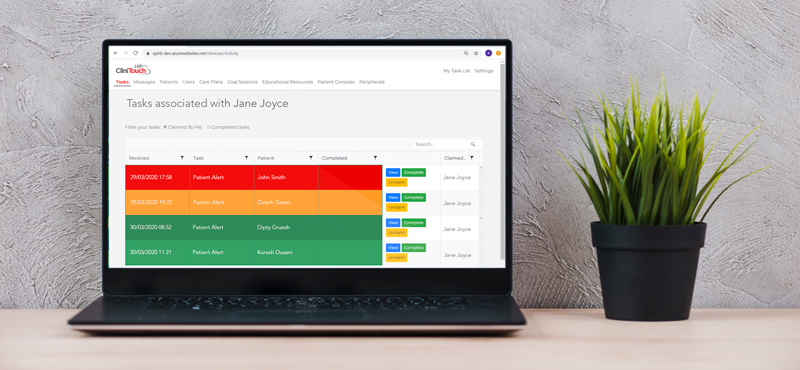
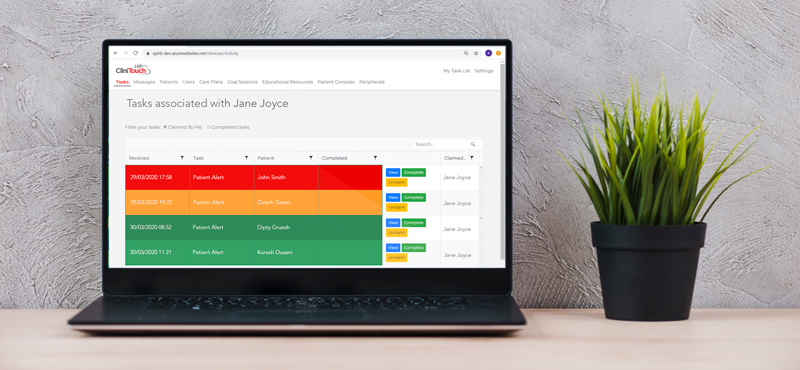
Dr Rama’s experience demonstrates exactly what our software is built to do. With a simple red/amber/green visual rating system, our software helps clinicians manage their caseloads more effectively, by identifying which patients are in urgent need of care and how they should be prioritised.
2. Some of my patients don’t have WiFi or own a smart device
Many patients have their own connected devices, and using a familiar tablet or smartphone is preferable. However, on our mission to make healthcare easier and more accessible, we can provide smartphones and tablets, as well as WiFi access, to any subscribed patient in need for the duration of the service.As highlighted in the NHS document on ‘Improving access for all: reducing inequalities in access to general practice services’, people with poor or no access to the internet often experience health inequalities and poorer outcomes1. To combat this, we can provide the necessary equipment and training to ensure our remote monitoring platform is accessible for all subscribed patients.Keeping patients digitally connected to their clinician, particularly if they live in a remote place and/or have poor access to local health facilities, enables their clinician to intervene when necessary to avoid unscheduled admissions and create better health outcomes.

3. I’m worried my patients will struggle to learn the software
We pride ourselves on offering a straight-forward, easy-to-use platform, that people of all ages and abilities can use. To ensure our users are having the best experience on our platform, our in-house development team work continuously with patients and clinical teams to improve the software based on their feedback.In fact, one of our patient users commented that “It’s extremely easy to use by someone who is not technically minded at all.”Although the platform is very easy to navigate, we do provide digital and paper guides to ensure users are confident with the software. Plus, our customer service team are available to help patients with any technical questions they might have.
4. I don’t have enough equipment to lend to patients to track their vitals
A crucial aspect of remote monitoring is patients being able to take their own vital readings, or a carer doing it on their behalf, for the data to then be passed onto the clinician. To facilitate this, we can lend the appropriate peripherals for the patient’s condition and train them how to use it. The patients can keep the equipment for the duration of the service. On this topic, clinicians sometimes question whether patients taking their own vital sign readings generates accurate data. A study exploring the feasibility of remote monitoring patients post elective surgery found that patients’ self-measurements of vital signs while using a remote monitoring system are comparable to that acquired by a nurse2.

5. My patients need educating on their conditions as well as monitoring
As well as tracking patients’ conditions, our remote monitoring platform CliniTouch Vie provides educational content to help patients take control of their health. We have a range of educational resources for people living with COPD and heart failure, and we are always adding new content for clinical pathways. This content can include images, diagrams, videos, audio files and written material. According to ‘See a voice’, the UK national reading age is nine years old3. The NHS highlighted that people with a low ‘health literacy’ levels are linked to a range of problems, such as inappropriate use of health services, general poor health, and reduced life expectancy4. Consequently, we designed all of our educational resources to be suitable for people with a reading age of nine so that the information is easily understood and more likely to have a positive impact on their lives.

6. It would need to be an integrated clinical system
We understand that clinicians don’t want multiple data sets in multiple places. With CliniTouch Vie, we can put the right data into the right place at the right time, and make it visible to the right team members. We are experienced in data sharing and can create a unified patient record to help clinicians communicate with one another.Our in-house development team gives us the capability to adapt to individual healthcare providers’ needs and ensure the software works in the best way for them.Our platform CliniTouch Vie is CE mark registered and we are Cyber Essentials Plus and ISO 27001 certified. This means we keep data safe and abide by European health, safety and environment protection regulations.
Need help breaking down your barriers?
Our team are experts in change management, stakeholder engagement, and co-designing solutions that stick. To find out more about how we can help you, get in touch at digital@spirit-health.com.
References
1 https://www.england.nhs.uk/wp-content/uploads/2017/07/inequalities-resource-sep-2018.pdf
2 Omar Faiz, Subramanian Nachiappan, Chukwuemeka Anele, Emma-Jane Roberts, Chris Barker (2018) ‘An observational study to assess the feasibility of remote monitoring of patients in the early postoperative period after elective surgery’, volume 4, issue 3, page 133-141
3 https://www.see-a-voice.org/marketing-ad/effective-communication/readability/
4 https://digital.nhs.uk/blog/transformation-blog/2019/creating-better-content-for-users-with-low-health-literacy.