By Sophie Davis-Cooper on March 4, 2021
Over the last twelve months, the NHS has been fundamentally reshaped. Plans and ideas that were bubbling away in the background for years suddenly received the green light by default. 2020 saw a huge increase in the adoption of digital technologies within modern healthcare economies.
From the adoption of video-based triage and GP-to-patient consultations within primary care, to remote monitoring for shielding and vulnerable patients, as well as those discharged early from hospital – both within their own homes and a care home setting, digital technologies have driven wide recognition that there is an alternative way to manage clinical caseloads within a primary setting.
 While this is unlikely to be a permanent shift, it is a seismic one. Yes, clinicians will – understandably – not want to manage their patients by video alone and there is no replacement for the face-to-face interaction within the privacy of a GP surgery. But, as of April 2021, NHS England will require all parts of our health and care system to work together as Integrated Care Systems (ICS), meaning that primary care is set to take a central role in providing joined-up care. Strategic commissioning will focus on population health outcomes. And digital and data will play an increasing role in placing citizens at the heart of their own care.
While this is unlikely to be a permanent shift, it is a seismic one. Yes, clinicians will – understandably – not want to manage their patients by video alone and there is no replacement for the face-to-face interaction within the privacy of a GP surgery. But, as of April 2021, NHS England will require all parts of our health and care system to work together as Integrated Care Systems (ICS), meaning that primary care is set to take a central role in providing joined-up care. Strategic commissioning will focus on population health outcomes. And digital and data will play an increasing role in placing citizens at the heart of their own care.
From providing educational resource to help empower patients to better manage their own conditions, to identifying and prioritising the patients that absolutely need to be seen and thereby easing the workforce burden faced by doctors, there is little doubt that digital will underpin primary care services well beyond the COVID pandemic. The adoption of digital solutions has shifted the paradigm about the way we will need to provide a proactive and preventative model of care in the future.

New mindset
Until March 2020, digital innovation was a consumer expectation that was largely unmet within UK healthcare. The old models of delivering care remained at odds with modern needs and possibilities. Patients wanted better ways of accessing healthcare and were increasingly demanding a voice and a choice in decisions about their care. The technology was there, but the challenge lay in getting innovation out there – and used – more effectively than we had done before.
What COVID-19 did was change innovation at a very local level, rapidly. Making headway during the pandemic relied on local healthcare economies building sensibly on what was already there. In the process, 2020 became the year when local health and care organisations used technology to help existing services work better and more efficiently; applying technological solutions to their current systems and pathways – giving patients and clinicians better access to information and education that would enable care to be delivered to those most vulnerable in the safety of their homes.
One of the major areas of technology adoption at a local and regional level has been in remote monitoring for the vulnerable: be those the frail and elderly within care homes; for those discharged early from hospital to free up COVID-19 beds; or those in the high risk category with long term conditions such as diabetes, heart failure or COPD.
By regularly and consistently monitoring these vulnerable patients, this technology allows GPs to triage their patients and know when to intervene. Extending the concept of care to one akin to a ‘virtual ward’, GPs get clinical information on their patients quicker and faster than they would do in the traditional setting which allows them to rapidly assess a patient, and better balance the dual aspects of risk management and time management.
This proactive model, centred around joined-up primary and community care, has allowed for early intervention that has helped keep people out of hospital, increased health system capacity and reduced the risk of cross contamination at a time when our collective focus has been on protecting our vulnerable and our NHS.
Improved collaboration for better outcomes
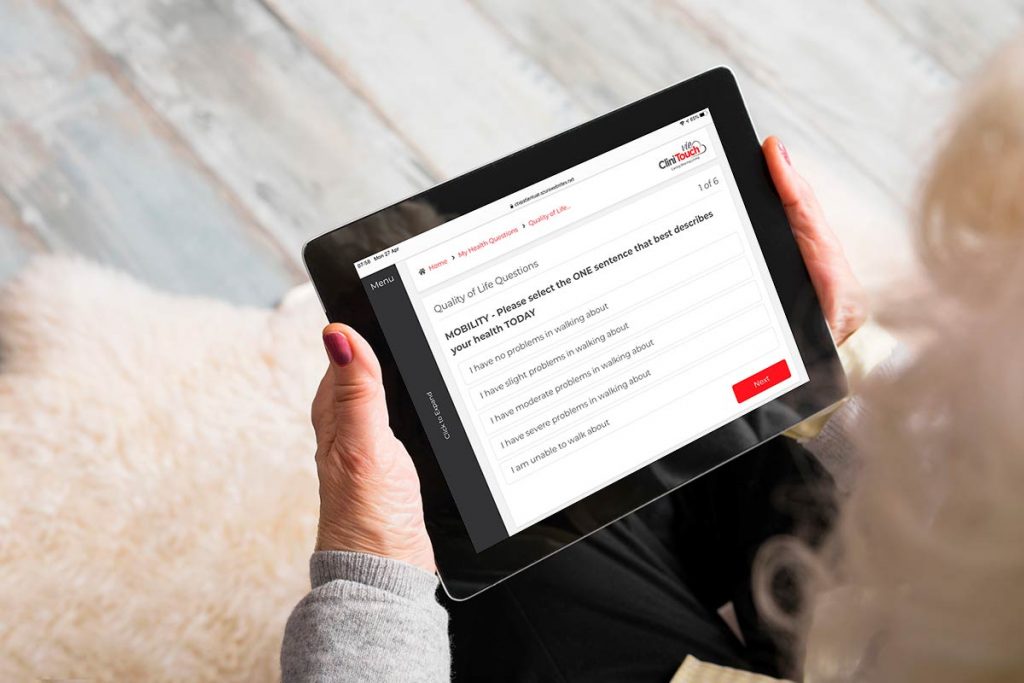
By connecting patients with their clinical teams from their own homes, patients are given much greater involvement in the management of their health, while healthcare professionals monitor their vital health information.
As a form of preventive care, remote patient monitoring puts everyday wellness at the forefront of patient care. It makes patients active participants in their healthcare by empowering them to willingly take control with the necessary tools and resources in place – from educational resources on their condition, to being aware of positive action they can take to prevent deterioration, and through better understanding of external factors such as air quality. When patients feel more involved in the process, it is more likely that they will become more invested in improving their health with their doctor’s guidance, allowing for a more collaborative experience for both parties.
The emerging evidence seems to suggest that patients of all ages are very adaptable to a digital approach, with high patient acceptability demonstrated on patient satisfaction questionnaires and the Family and Friends Test (FFT). It is likely that the need for patients to feel COVID-secure within their homes whilst still having the confidence that they are connected to their clinicians has increased their openness to the adoption of digital solutions. However, there is a balance between letting the technology dictate the digital solution whilst communicating the benefits and useability of the technology for both patients and clinicians.
In parallel, the pandemic has also shown the value of real-time collaboration between GP practices and an entire network of healthcare providers to ensure the right patients are treated at the right time. From the nurse practitioners and pharmacists that play a key role within practices, to the hospital consultants, care homes, opticians and dentists, the concept of working together as a team to look after patients – in addition to how patients themselves can also contribute positively to their own care – is now firmly established.

Looking beyond COVID
There is no doubt that health care has seismically changed during 2020. Yet, gaps remain if we are to reach NHS England’s vision of a truly joined-up, proactive and preventative service with citizens at the heart of their own care.
Firstly, we have to ensure healthcare is more digitally inclusive – and that requires infrastructure and education. The priority for 2021 is to address the technology gaps revealed by the COVID-19 NHS response and to use that knowledge to achieve a wider adoption of a broad, effective community care model within local health economies.
“Local health economies have to move from a mindset where we have a portfolio of individual technical projects, to having a strategic, joined-up digital transformation programme that is based upon making healthcare accessible for all; easy to navigate; and centred around the individual needs of a patient – or carer – within their own care setting. This means having a system that isn’t based on the physical location where patients access care, but extending care into a remote, virtual model, empowered by technology.”
– Nicola Haywood-Alexander, Chief Information Officer, NHS Lincolnshire STP
The second challenge is around harnessing data. With the increased adoption of digital technology comes data that can be analysed, using machine learning and artificial intelligence, to help us not just identify in real-time those patients who need priority care, but also predict those who are more at risk, from either physical or psycho-social conditions.
It will enable us to look at trends; to better understand the side effects of medication on specific cohorts of patients. It will provide insight to help us better understand mental health, as well as making it much easier to carry out research and develop therapies. And moreover, it will enable us to gain early detection of potential future pandemics through the raising of warning flags in the system.
Conclusion
Under the most strenuous of circumstances, great strides forward have been made in digitalising healthcare and transforming many care pathways from the traditional, reactive model to one focused on prevention and pro-active care.
This is a once in a generation opportunity for change. As we look ahead beyond COVID-19, it is imperative that policy makers, clinical leaders and front line staff maintain their grasp on the digital opportunity and begin business better than usual today.
To find out more about how we can help you deliver remote monitoring for your patients, please get in touch by email at digital@spirit-health.com.


